ABCs of Andrés
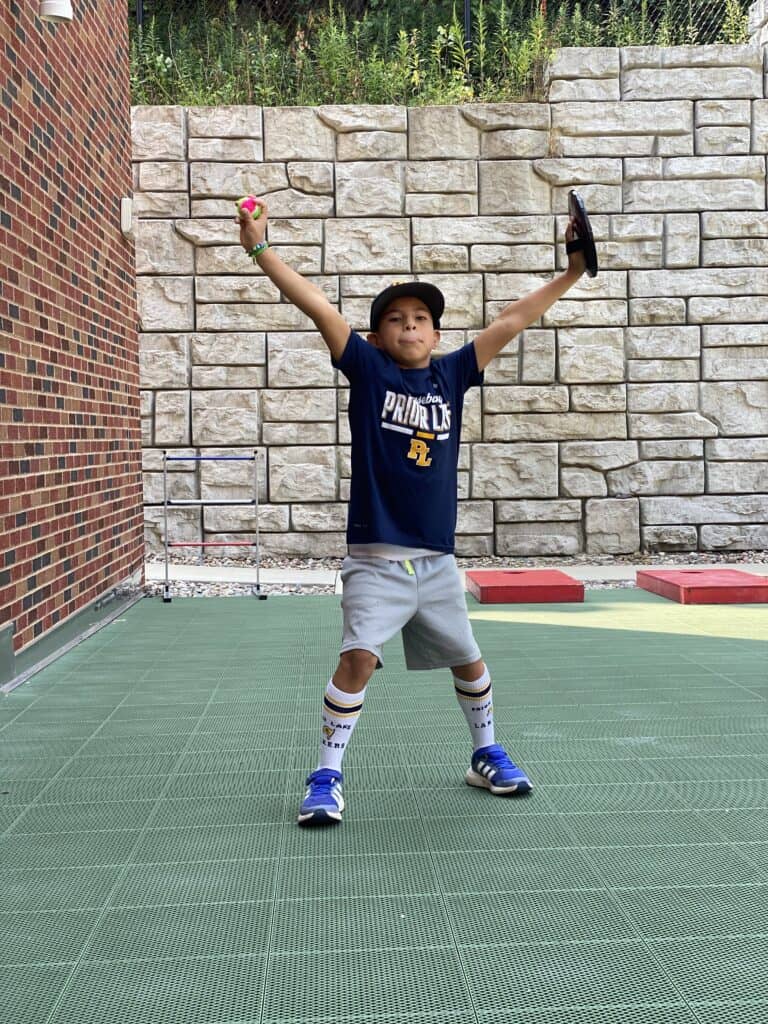
Andrés was adopted from Bogotá, Colombia, when he was 21 months old, but that was the least astonishing part of his journey. Katie and James expected a six-week trip to the South American country, but weeks turned into months, as…
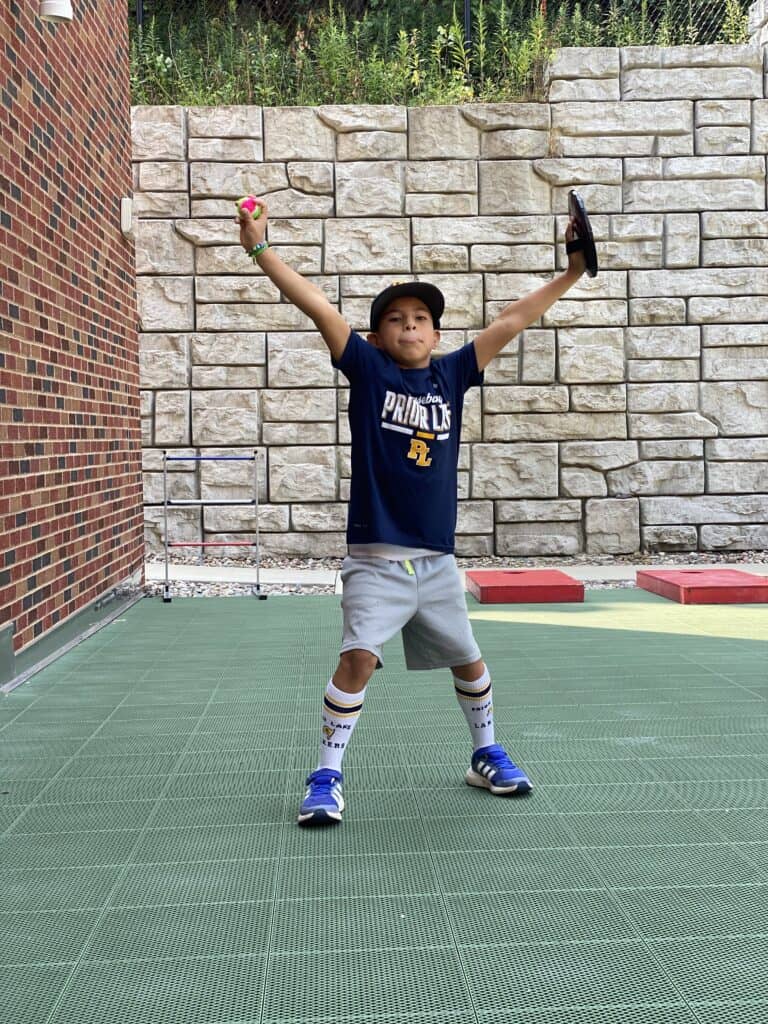
Andrés was adopted from Bogotá, Colombia, when he was 21 months old, but that was the least astonishing part of his journey. Katie and James expected a six-week trip to the South American country, but weeks turned into months, as…

Every year on rare disease day, every front porch in a small Minnesota town is illuminated by purple lights…and every light is for Everleigh. Everleigh, or Evie, was born early by caesarean section—36 weeks and six days. As far as…

Waylon was born 10 weeks early at 1 pound, 8 ounces, and 12 inches long. He had already persevered; now he needed to grow. When Kari and Josh learned she was pregnant with their third child, they approached it differently;…

Parents rarely feel prepared for twins. They feel even less prepared when the twins are born four months early. Ashley and DJ were ecstatic when they found out she was pregnant. They were even more ecstatic when they found out…

As Laura glanced at her phone, it started ringing… It was their doctor’s personal cell phone. “We just accepted a heart for Bianca.” The call ended a three-year journey for Bianca…and started the rest of her life. Life was relatively…

It’s a Minnesota family’s dream: a Hawaiian vacation to escape the winter cold. But for Jill and Greg…it quickly turned into a scary and stressful reality. Greg’s parents were celebrating their 45th wedding anniversary and paid for all their kids…

Despite being born at 34 weeks, Alejandro was normal size and had no lingering medical concerns. Seven months later…he was on his way to the United States. “As his mom, I could feel it,” said Adriana. “Something was wrong.” Doctors…

Surprises are generally good, but when Ethan was born…it was a challenging surprise for him and his parents. “You can’t see it on an ultrasound,” said Kim, Ethan’s mom. Doctors in our hospital had never seen anything like it. No…

Javohn and his dad, Thomas, did not expect such a long and difficult journey. But after two tumors and one year of radiation and chemotherapy…it is almost time for Javohn to rejoin his five siblings in Belize. “He is a…

Jesus and Leamsie have two beautiful sons: Elian and Adrian. And after spending 323 nights at the Ronald McDonald House of Rochester, Minnesota…they are thankful for every day they have together. Elian, their oldest, was diagnosed with a cancerous brain…